Alzheimer’s disease is a progressive brain disorder and a form of dementia that affects memory, thinking, and behaviour. As symptoms become more severe, the disease can seriously affect a person’s ability to perform tasks that would otherwise be deemed routine, like brushing teeth, making a meal or even recognising family members.
For many years, the leading theory has been that Alzheimer’s is caused when two harmful proteins called amyloid-beta and tau accumulate in the brain. This pile-up sets off a chain of events, eventually damaging nerve cells and leading to memory loss, confusion, and mood changes. This destruction doesn’t happen overnight. It begins years, even decades before symptoms appear.
In 2021, an estimated 57 million people worldwide were affected by dementia, with Alzheimer’s contributing to 60-70% of the cases. Currently, there is no cure for Alzheimer’s but there are treatments that can slow symptoms and improve quality of life.
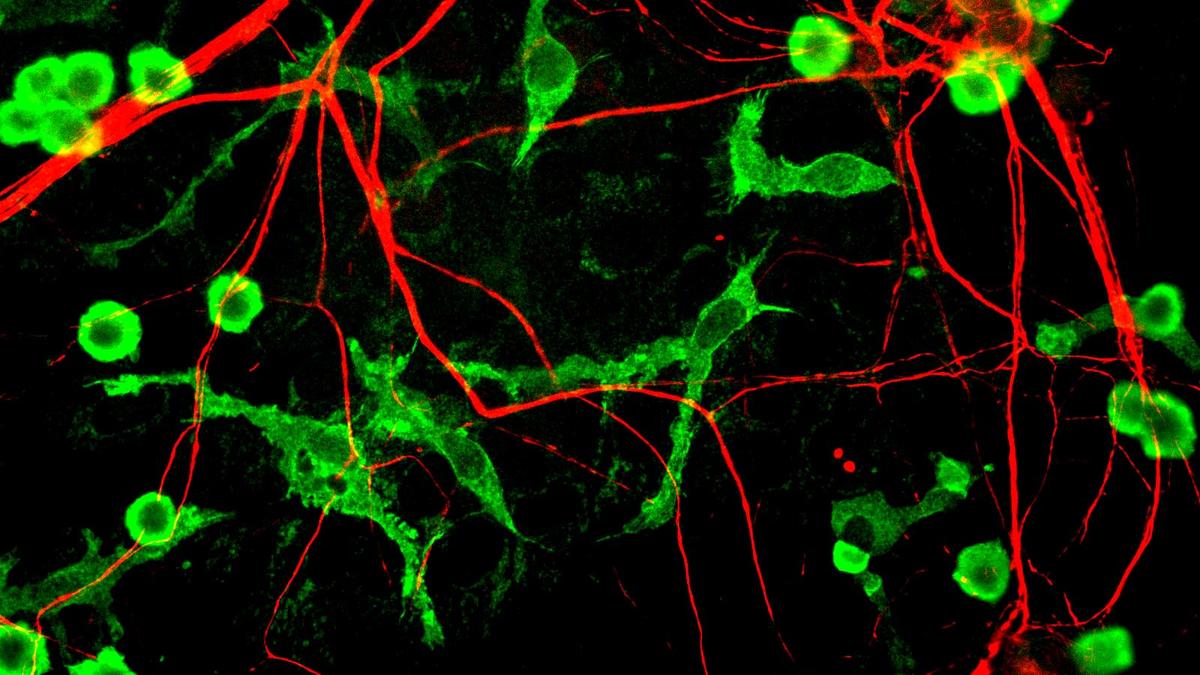
It isn’t surprising that in the ongoing search for answers, scientists are increasingly turning their attention from neurons to their lesser-known but equally critical neighbours: microglia, the brain’s resident immune cells.
In a new study published in Immunity, researchers led by Gaurav Chopra at Purdue University have uncovered how fat metabolism in microglia may be a key driver of disease progression.
“This study is pretty interesting and part of a growing body of studies indicating the role of fat metabolism problems in cells around amyloid plaques,” Indian Institute of Science professor Deepak Nair said.
The lipid link
In healthy brains, microglia serve as surveillance cells, clearing away waste products and toxic proteins like amyloid-beta (Aβ), the sticky molecule that forms the hallmark plaques in Alzheimer’s. This clean-up process helps protect neurons from damage. But in Alzheimer’s patients this mechanism fails.
“The big question was: how and why are microglia no longer able to eat up or clear these plaques?” said Priya Prakash, a co-lead author of the paper. “This isn’t a new observation. Dr. Alzheimer himself noted fat vacuoles in glial cells over a century ago, but their functional significance has remained unclear until now.”
The study identified DGAT2, an enzyme that converts free fatty acids into triacylglycerols (TAGs), the main component of lipid droplets, as a key player. In both mouse models and post-mortem human brain samples from patients with late-stage Alzheimer’s, the researchers found that microglia near amyloid plaques have high DGAT2 expression and are bloated with lipid droplets, particularly in the hippocampus, the region responsible for memory.
“We see that the proximity of microglia to plaques correlates with lipid droplet size. The closer they are, the fatter they get,” Prakash noted.
What causes the lipid overload? According to the study, Aβ exposure triggers a metabolic chain reaction. Microglia start converting free fatty acids into fats stored inside lipid droplets. Over time, this lipid build-up disrupts their ability to engulf and digest more Aβ, setting up a vicious cycle: more plaques lead to more fat, which leads to more dysfunction.

The research team used advanced imaging, lipidomic analysis, and metabolomics to track how microglia’s lipid profiles changed over time in response to Aβ exposure. Initially, microglia accumulated toxic free fatty acids. Later, with the help of the DGAT2 enzyme, they converted these fatty acids into triacylglycerols and stored them in lipid droplets.
To test whether this lipid build-up could be reversed, the researchers used genetically engineered mice that mimicked human Alzheimer’s, known as 5xFAD mice. Two methods were used to reduce DGAT2 activity: a pharmacological inhibitor, currently in clinical trials for non-alcoholic fatty liver disease, and a custom-designed PROTAC-like degrader that targets DGAT2 specifically in microglia.
“When we blocked DGAT2, we saw reduced fat accumulation in microglia and restoration of their ability to clear amyloid plaques. Even a one-week treatment in aged mice with heavy pathology drastically reduced the plaque burden by over 50% and significantly reduced neuronal damage markers,” Prakash said.
However, Prof. Nair cautioned that the animal model used in this study is an accelerated Alzheimer’s disease model that relies on Aβ pathology, so the findings may not be equally applicable to all forms or stages of the disease.
A fat-filled puzzle
Lipid droplets are not inherently bad. In fact, they help cells survive stress by safely storing excess fat. But in microglia that are chronically exposed to Aβ, this once-protective response turns harmful. The study’s authors suggested that microglia sacrifice their protective immune function in exchange for lipid safety and that this trade-off may be a key step in Alzheimer’s progression.
The study also uncovered a notable sex-based difference: female mice accumulated more lipid droplets in their microglia and showed more severe microglial impairment than males. This echoed real-world data that show women face a higher risk of developing Alzheimer’s.
Because DGAT2 is expressed in many cell types throughout the body, targeting it systemically could lead to unwanted side effects. The team’s microglia-specific degrader represents an early but promising step towards cell-selective therapy.

“This is a beautiful proof of concept,” Prof. Nair said. “We’ve had over 100 drugs in clinical trials for Alzheimer’s in the past 20 years, and very few have succeeded. The disease is complex in its origin — it’s not caused by one thing.”
While the amyloid cascade hypothesis has dominated the field for decades, more recent theories incorporate inflammation, tau protein tangles, metabolic dysfunction, and now, lipid metabolism.
“In brain diseases, homeostasis slowly breaks down until the system is overwhelmed,” Prof. Nair said. “If we can control just three or four critical pathways, lipid metabolism being one of them, it might be enough to slow down that collapse.
“And slowing down matters. A five-year delay in Alzheimer’s onset would significantly reduce the socioeconomic burden of the disease.”
Manjeera Gowravaram has a PhD in RNA biochemistry and works as a freelance science writer.
Published – July 13, 2025 05:00 am IST