In 2023, malaria infected nearly 294 million people and killed close to 6,00,000. Despite early victories in the fight against malaria, global progress has stalled in recent years. The parasites are adapting, becoming resistant to treatments, while mosquitoes are surviving insecticides. It’s a shape-shifting enemy—and the old tools are slipping.
India has reduced its malaria burden by over 80% between 2015 and 2023—but last year, tribal districts such as Lawngtlai (Mizoram) and Narayanpur (Chhattisgarh) still recorded malaria rates of over 56 and 22 cases per 1,000 people, respectively as per the National Centre for Vector Borne Diseases Control —reminders that the parasite continues to thrive in several pockets long after national averages have improved.
While Africa faces mostly Plasmodium falciparum, India also battles the relapse-prone Plasmodium vivax which can lie dormant in the liver and reawaken weeks or, even months later. In Jharkhand, mixed infections account for nearly 20% of cases (NCVBDC), complicating elimination. Even where incidence has dropped, the parasite can persist—lurking in asymptomatic carriers (people with no symptoms) or returning months after infection.
The search for smarter, longer-lasting vaccines has never been more urgent.
Hope with limits: RTS,S and R21
After decades of setbacks, the first approved malaria vaccine—RTS,S—arrived in 2021. It offered about 55% protection in the first year, but efficacy waned by 18 months, requiring a fourth booster dose.
The R21/Matrix-M vaccine, developed by Oxford and the Serum Institute, showed up to 77% efficacy in Phase 3 trials winning World Health Organization (WHO) approval in 2023. Fewer doses, low cost, and Indian production make it especially promising.
Still, both vaccines target only one stage of the parasite, leaving reinfection and transmission a lingering threat.
Whole-parasite vaccines: a stronger shot on the horizon
Instead of targeting a single protein, like in RTS,S and R21, whole-parasite vaccines expose the immune system to the entire malaria parasite—alive, but weakened. The experimental PfSPZ vaccine mimics natural infection using radiation-weakened P. falciparum sporozoite (the parasite’s early-stage form) delivered directly into the bloodstream. Early studies showed that 96% of participants developed strong antibodies, with up to 79% protection after the third dose.
Building on that foundation, a modified version called PfSPZ-LARC2, developed by Sanaria, may push efficacy even further. The simplicity of a one-dose regimen, despite the intravenous requirement, could make it a strong candidate for targeted use in outbreak zones or among hard-to-reach migrant populations in India.
Unlike vaccines that target the parasite’s earlier stage, PfRH5 acts during the blood stage, when symptoms appear and the risk of severe illness increases. Since RH5 is a vital protein for red blood cell invasion that the parasite can’t easily alter, it offers cross-strain protection—a rare asset in malaria vaccine design. Phase 1a/b and Phase 2b trials in the UK, The Gambia, and Burkina Faso have shown promising outcomes. These vaccines could complement earlier-stage ones and may help boost natural immunity in people who’ve previously had malaria.
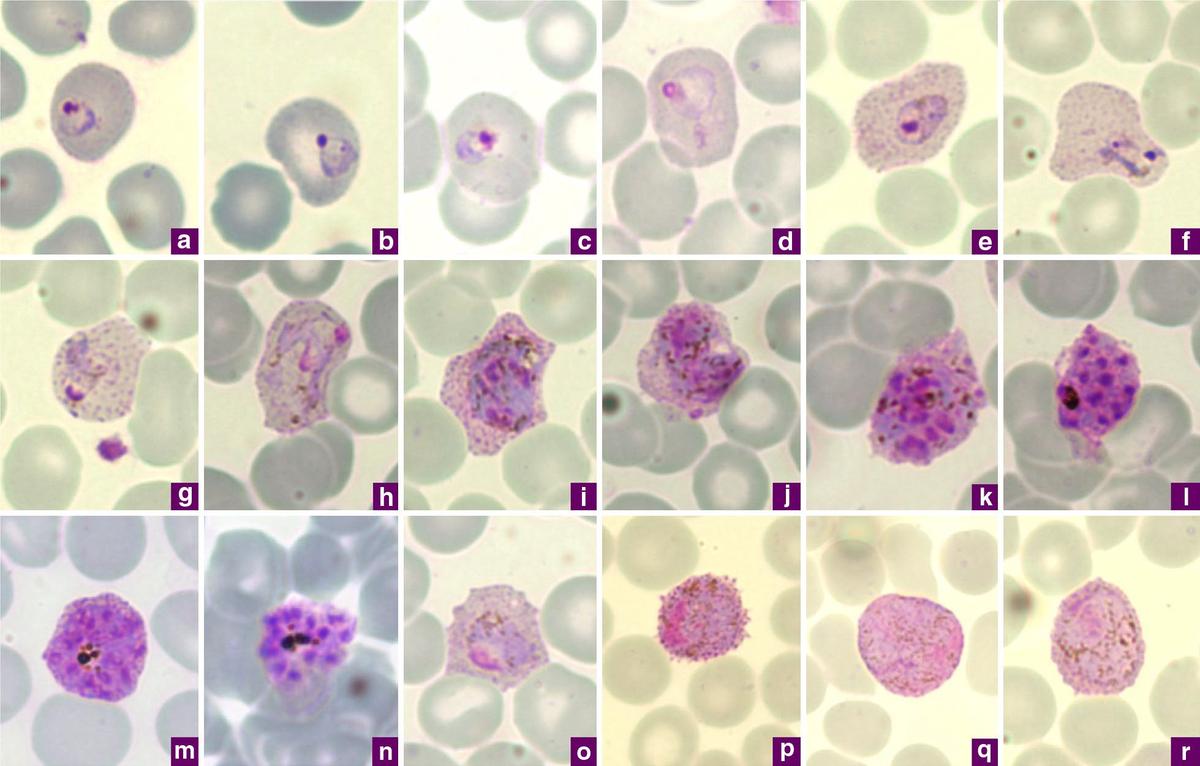
Photomicrographs of Plasmodium vivax in Giemsa-stained thin blood films
| Photo Credit:
By Chavatte JM, Tan SB, Snounou G, Lin RT – Chavatte JM, Tan SB, Snounou G, Lin RT (2015). “Molecular characterization of misidentified Plasmodium ovale imported cases in Singapore.”. Malar J 14: 454. DOI:10.1186/s12936-015-0985-8. PMID 26577930. PMC: 4650842.- “This article is distributed under the terms of the Creative Commons Attribution 4.0 International License(https://creativecommons.org/licenses/by/4.0/)“, CC BY 4.0, https://commons.wikimedia.org/w/index.php?curid=122024897
Transmission-blocking vaccines
While the above vaccines aim to protect individuals, transmission-blocking vaccines (TBVs) target the parasite in the mosquito—halting its spread at the population level. Pfs230D1 induces antibodies that prevent parasite fertilization within the mosquito gut. In Mali, it reduced transmission by 78% in a Phase 2 trial.
This strategy is especially relevant to India with a far higher proportion of asymptomatic carriers. “Our group and others in India are actively working on TBVs to address this reservoir,” said Agam P. Singh, scientist at the National Institute of Immunology, New Delhi.
India, too, is entering the TBV space with its own candidates. In July 2025, AdFalciVax was announced by the Indian Council of Medical Research (ICMR), the country’s first indigenous dual-stage malaria vaccine. Unlike single-phase vaccines, it combines pre-erythrocytic (PfCSP) and transmission-blocking (Pfs230 and Pfs48/45) antigens to both prevent infection and block mosquito transmission. “AdFalciVax has completed preclinical testing,” said Subhash Singh, who leads the programme at ICMR-RMRC Bhubaneswar. In mice, it triggered strong immune responses lasting over four months—roughly equivalent to a decade in humans—and remained stable at room temperature for nine months, potentially aiding rural deployment.
Progress is also visible beyond P. falciparum. A first-in-human trial in Thailand showed that the P. vivax TBV Pvs230D1M reduced mosquito transmission by up to 96%, another ray of light for India’s mixed-species numbers. India, too, is not far behind. “A similar research program for P. vivax is underway, in collaboration with AdFalciVax co-inventors Sanghamitra Pati and Sushil Singh,” said Dr. Singh.

Boosting immune power
Strengthening the immune response itself is another active front. A recent protein-based vaccine combined a ferritin nanoparticle with CpG—a type of adjuvant, or immune booster already used in hepatitis B vaccines—and cut liver-stage parasite burden by 95% in mice.
AdFalciVax showed over 90% protection in mice even with alum, a mild and widely used adjuvant. “We saw protection on a par with more inflammatory adjuvants such as MPLA (a stronger adjuvant),” said Dr. Singh. “Whether this holds in humans remains to be seen.”
Scientists are also testing newer vaccine platforms such as mRNA, which allow vaccines to be made faster and tweaked more easily than protein-based ones. In 2025, researchers at CureVac and the U.S. National Institute of Health (NIH) encoded the Pfs25 antigen—targeting the parasite’s sexual stage—into an mRNA-lipid nanoparticle. They observed complete transmission blockage in mice, with antibodies lasting over six months from just two doses.
However, not all mRNA-based vaccine efforts are moving ahead smoothly. In early 2025, BioNTech’s Phase I/IIa trial for its blood-stage mRNA vaccine candidate BNT165e was placed on clinical hold by the U.S. Food and Drug Administration (FDA). While the company did not disclose the reason, it noted that discussions with regulators are ongoing. The pause highlights the hurdles of translating mRNA platforms into malaria vaccines.
“mRNA and nanoparticle platforms can certainly be explored—alone or in combination,” said Pawan Malhotra, emeritus scientist at the International Centre for Genetic Engineering and Biotechnology (ICGEB), New Delhi. “But it’s hard to predict what will work. Plasmodium is complex, unlike bacteria or viruses.”

A nurse administers a malaria vaccine to an infant at the health center in Datcheka, Cameroon January 22, 2024. File photograph
| Photo Credit:
REUTERS
Augmenting existing vaccines, blocking immune evasions
Beyond boosting the strength of the immune response, scientists are also exploring how to improve its aim—modifying malaria antigens to help the body recognise the parasite more efficiently. A new experimental vaccine links PfCSP—a surface protein from the malaria parasite—to MIP3α, a molecule that acts like a flare to draw in immune cells. In mice, it triggered stronger antibody and T cell responses than standard mRNA vaccines, reducing liver-stage infection by up to 88%. It hasn’t yet been tested in humans, but it shows how tweaking the immune response could push malaria vaccines past current limits.
Beyond vaccines, researchers are exploring how malaria hides from our immune system. P. falciparum uses RIFIN proteins to bind to immune ‘off switches’ like the LILRB1 receptor, shutting down immune cells.
It’s a tactic that helps the parasite hide in plain sight.
A new study describes an experimental, engineered antibody, D1D2.v-IgG, designed to block this interaction. Built from a segment of the LILRB1 receptor, the antibody binds to RIFIN 110 times more strongly than the natural version—outcompeting the parasite at its own game. By blocking this interference, it freed the body’s LILRB1 to function normally, restoring immune attack in lab tests. Though still untested in animals, the approach could one day support new malaria therapies or enhance vaccine responses.
Gene drives and vector suppression
While engineered antibodies attack the parasite, CRISPR-based gene drives go after its vector. These tools insert fertility-disrupting genes into mosquitoes. In a landmark study, this approach wiped out entire Anopheles gambiae colonies within a year—with no resistance detected.
But evolution rarely plays along. In the wild, mosquitoes might adapt, ecosystems could shift, and once released, gene drives can’t be recalled. The idea of eradicating a species raises thorny ethical and ecological questions.
So, researchers are exploring subtler strategies. One 2025 study edited a single letter in the FREP1 gene, blocking the malaria parasite from developing inside the mosquito. With a gene drive, this parasite-blocking trait spread to over 90% of lab mosquitoes in ten generations—without harming their fertility or survival. But the parasite remains under pressure to evolve around the block, and infected mosquitoes still live long enough to potentially transmit malaria if the trait doesn’t saturate the population.
Another team took a different route—engineering mosquitoes to die sooner only when infected. By disabling an immune gene, they created a self-limiting feedback loop: the more malaria spreads, the more it kills its own carriers. Because this strategy doesn’t attack the parasite directly, it reduces the pressure for resistance. It’s an elegant inversion—using the parasite’s success against itself to shrink transmission, without eradicating the vector or requiring perfect coverage.
The Indian lens: challenges and the path ahead
The nation aims malaria elimination by 2030. It’s an ambitious plan—but one that hinges on precision and persistence.
Tribal and forested districts in Chattisgarh, Jharkhand and parts of the Northeast are the last strongholds of malaria—often remote areas with limited healthcare access. Even in places where infections seem to be minimal, adults and older children often act as asymptomatic reservoirs, quietly sustaining transmission.
A municipal worker sweeps the road in front of a wall painting that depicts Sir Ronald Ross, known for demonstrating that the Anopheles mosquitoes transmit the Plasmodium parasite, providing the first evidence-based explanation of malaria transmission
| Photo Credit:
KVS GIRI
The dual-species landscape in India further complicates elimination efforts.
“P. cynomolgi—a monkey malaria species—is the best model for P. vivax research,” said Dr. Malhotra. “We were developing it 20 years ago with the Central Drug Research Institute (CDRI), but strict monkey access laws and lack of scientific foresight stalled it.”
Despite these challenges in vivax research, efforts to develop a vaccine are gaining ground. Both Dr. Subhash Singh at ICMR and Dr. Agam P. Singh at NII confirm that P. vivax vaccine candidates are under active development.
But even the most innovative science needs systems to carry it forward.
“We need a COVID-style push,” said Dr. Malhotra. “Industry and academia must collaborate with proper funding. We’ve developed potent therapeutic antibodies against liver-stage parasites and now need partnerships to move them forward. A lone scientist in a lab can’t do it all.” The science is advancing—but it needs infrastructure and political will to match.
Dr. Singh echoes the sentiment. “We are now concentrating on translating AdFalciVax’s promising preclinical results into trials. Successful deployment however, will require good results over multiple stages of trials as well as regulatory approvals, likely taking at least 7–8 years.” In addition, strong coordination between regulators, industry, and researchers is needed. ICMR has already floated an Expression of Interest seeking industrial partners to co-develop the vaccine. “Challenges that need to be addressed include producing GMP-grade components, developing immune biomarkers, and benchmarking efficacy against RTS,S and R21,” added Dr. Singh.
“We definitely need vaccines, antibodies, new drugs—for both P. falciparum and P. vivax,” said Dr. Malhotra. “But that’s not enough. Doctors need training, resistance must be tracked, and vector control has to keep pace.” It must be a full-spectrum battle—from the molecular level to the community clinic.
India’s malaria story is no longer one of uniform burden—it’s a fight against hidden reservoirs, remote geographies, and a parasite that won’t quit. With next-gen vaccines, homegrown innovation, and growing scientific momentum, the country stands at a critical juncture. Elimination by 2030 is not just a goal—it’s a test of whether science, policy, and public health can unite to defeat an ancient foe. The tools are here. Now, we must use them—decisively and everywhere the parasite still survives.
(Anirban Mukhopadhyay is a geneticist by training and science communicator from Delhi. [email protected])
